Spotlight
The evolution of mental health care over 75 years
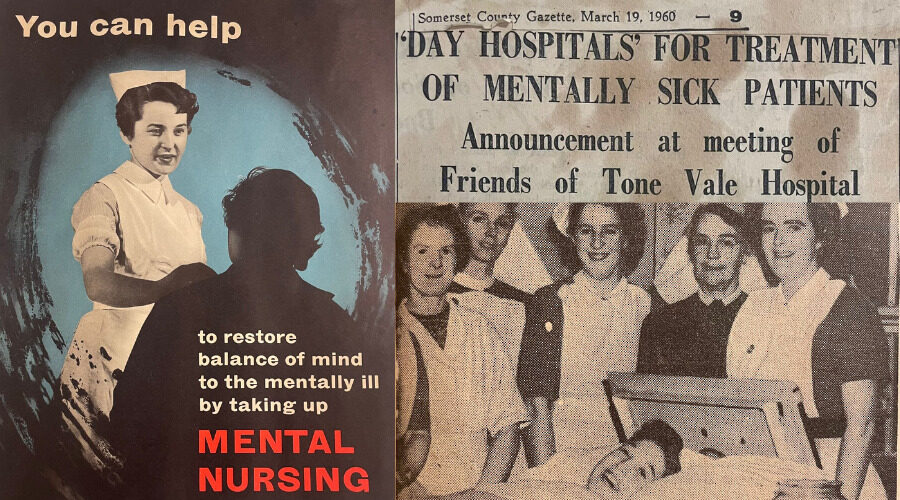
It was only 75 years ago that the term 'mental health' conjured up much different connotations than it does today. People with mental health issues were referred to as ‘the mentally sick’, and were sent to sanatoriums or asylums to be treated for their disorders. Society has come a long way since then, with the stigma around mental health being challenged every day, while the way we deliver mental health services has rapidly evolved.
Our associate medical director for mental health and learning disabilities, Dr Andreas Papadopoulos, reflects over the changes in mental health care, and the advancements we’re making here in Somerset…
How mental health care has evolved - Andreas Papadopoulos
The world has changed significantly over the last 75 years, with the introduction of motorways, mobile phones, space travel, and artificial intelligence. And with all the global technological changes, so have our attitudes and our lifestyles, causing a change in our health care needs too. The NHS has had to adapt to these changes and provide appropriate healthcare that matches the ever-changing demands of the population, promoting better health and better quality of life.
When it comes to mental health, perhaps the biggest change has been the shift in people’s attitudes, and an understanding and acceptance around mental illness. With this improved acceptance – although more work needs to be done to fully destigmatise mental illness – people have been more able to talk about their mental health and seek help when needed. As a result, we have moved from the traditional and more feared diagnoses of schizophrenia, bipolar affective illness, depression, and anxiety, to a new understanding of the mental health problems that people are faced with.
We are now looking at mental health not only from a biological perspective, but also through the lens of social and psychological makings. New diagnoses have been developed with their own distinct diagnostic criteria, along with other neurodevelopmental and neurodegenerative disorders.
This shift in societal attitudes has inadvertently affected the legal framework available in the UK for the treatment of people with mental illness. Since its original inception and legalisation, the Mental Health Act is now yet-again changing to take into account the changes in the health care system, such as the closing of the asylums and the moving of care into the community, putting the pressure on professionals to always try and follow the least restrictive pathway of treatment. It is now looking to better protect people with autism and learning disability, ensuring that they continue to receive the best possible care while protecting their human rights and their quality of life.
As our understanding changes, so have the treatments we can offer. We have new medications, and we have taken advantage of the technological progress made and managed to develop less invasive treatments such as repetitive Transcranial Magnetic Stimulation (rTMS) for the treatment of depression.
There has also been a significant increase of different psychological or talking therapies offered, and improved access to these services. Not all mental illnesses require medical input and medication, and psychologists have supported the development of bespoke therapies. Dialectical behavioural therapies, cognitive behavioural, and analytical therapies are now widely available through local health care providers, together with family therapy and others. This increase in talking therapies has had a hugely positive impact on patients, with people learning to better understand their own mental health needs and how to best address them, while reducing the stigmatisation of mental illness and promoting acceptance.
In Somerset we have tried to follow suit with all the changes around mental health care, and in many ways have also acted as trailblazers for improved access to support available for people experiencing problems with their mental health. We have improved our community services, including our home treatment team and our first response service, which are geared to treat people at home and reduce the need for admissions, which would disrupt their daily lives and remove them from their supportive circle of family, friends, and other loved ones.
But we have also realised that in order to reach as many people as possible, we could not do it by ourselves. For that reason, we partnered with the voluntary and third-party sectors to establish Open Mental Health – a national first. Open Mental Health is a collaboration of voluntary, third-party sector, and specialist NHS services, working together to improve access to support for all people in Somerset who may require it. Together we have managed to bridge the gap between primary and secondary care, and allowed people that do not necessarily require specialist support, to still receive help when struggling with their mental health. Even more than that, if their problems persists and specialist assessment and treatment is required, the door is already open for them.
We have also set up the Recovery College which provides a wealth of courses and activities aimed at improving people’s mental health and access to local communities. We recognise that for people to have a meaningful and fulfilled life, they need to be part of their local communities and the Recovery College can support people with building up the skills and confidence in doing so, while offering them support and advise along the way.
Despite our above initiatives, we recognise that certain populations in Somerset, such as rural farming and travelling communities, are difficult to reach. To combat this, we have been actively reaching out to these communities, building trusted relationships that can improve access to our services and making support accessible to all.
Recognising the impact of depression on the people of Somerset, we have established a new difficult-to-treat depression pathway. We are one of the very few trusts in the country that is able to offer rTMS and vagal nerve stimulation to patients who've suffered with depression, but have not responded to traditional medication and psychological interventions. We've also established a new pathway for the assessment and treatment of people with ADHD, a diagnosis that has so rarely been monitored in the past, leading to problems at school, work, and life in general for those people with later comorbidities resulting in anxiety, depression and even substance misuse.
But this is not where we stop. Population needs are constantly changing, and we remain committed to improving and changing our services to reflect the local needs. And we do this by working with experts by experience. We are lucky to have colleagues who are enthusiastic, knowledgeable, and committed to helping the people of Somerset enjoy better mental health, but it is our experts by experience – people from Somerset who have experienced issues with their mental health themselves who can really tell us what is needed and how best delivered – that can help us to modernise and strengthen our mental health systems, through collaboration and co-production.
This is my cue to say a big thank you to everyone working within our mental health services in Somerset! Together we can continue to move far away from the stigmas facing people when the NHS was first introduced, creating a more accepting and accessible service for everyone.

